Stroke case study
Mr. S. is a 23-year-old man who sustained a traumatic brain injury as an unrestrained driver in a motor vehicle crash. On admission, his blood pressure (BP) was 158/72 mm Hg, heart rate (HR) 46 beats per minute, respiratory rate (RR) 28 breaths per minute, and temperature 96.2o F (35.6o C). His neurological examination reveals that his right pupil is at 6 mm and reacts sluggishly; his left pupil is 4 mm and reacts briskly. He is nonverbal, extends his arms bilaterally to pain, and opens his eyes minimally to pain. He is quickly intubated and placed on mechanical ventilation. A computed tomography (CT) scan is ordered, which reveals a large right subdural hematoma with cingulate herniation from right to left, as well as right-sided uncal herniation.He is taken to surgery emergently for a craniotomy to remove the subdural hematoma. After surgery, he arrives in the critical care unit with a ventricular catheter to measure intracranial pressure (ICP). His initial ICP is 24 mm Hg, BP 130/67 mm Hg, mean arterial pressure (MAP) 88 mm Hg, HR 54 beats per minute, RR 12 breaths per minute (controlled ventilation), and temperature 96.1o F (35.5o C). His current Glasgow Coma Scale (GCS) score is 3, but the anesthesiologist did not reverse the anesthesia, choosing to allow it to wear off gradually. He has orders for 3% saline at 20 mL/hr intravenously.QuestionsBased on the information provided, what is Mr. S.’s preoperative GCS? What is the significance of this number, and how would the nurse describe this to his family?Anatomically, what is the cause of his pupillary changes?Which of his postoperative findings are of concern?Why is the 3% saline ordered, and how will the nurse know if it is effective?
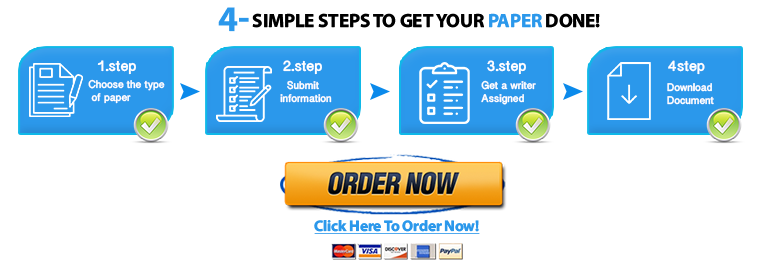
"Looking for a Similar Assignment? Order now and Get 10% Discount! Use Code "Newclient"